ACD-CPR & the rise of the machine?
If conventional cardiopulmonary support (CPS) in cryonics is difficult to perform adequately, and impossible to sustain for more than brief periods (30-60 min) before exhausting even a 3-man standby team, this is even more the case for active compression-decompression CPS (ACD-CPS) using the ResQPump (formerly the Ambu CardioPump). Even in the conventional medical setting of comparatively brief periods of CPR before defibrillation ACD-CPR is difficult to do, let alone do well. Indeed, if ACD-CPR (in conjunction with an impedance threshold device such as the ResQPod) continues to show superior results in terms of outcome (as it is now doing in recent and ongoing clinical trials) it may be the advance that makes heart-lung resuscitators both medically acceptable and cost effective. There is some evidence that this may actually be happening; while not yet profitable, the LUCAS CPR device is gaining in popularity and continues to be the subject of consistently favourable laboratory and clinical studies.
Currently, mechanical CPS is viewed by paramedical personnel as not just dangerous (i.e., the myth of routinely broken ribs and lacerated lungs and livers) but also as ineffective and, perhaps just as importantly, as a potentially professionally demeaning or threatening piece of technology. In my 30 years of experience interfacing with EMTs and paramedics in both the US and UK regarding mechanical CPR, the most frequent remark I’ve heard is, “I can do better CPR than that machine can.” Since CPR is the most dramatic, and arguably one of the most defining practices in emergency medicine, it is perhaps understandable that many emergency medical system (EMS) personnel will equate replacement of manual CPR as equivalent to replacement of the people who perform it. Many paramedics perceive the heart-lung resuscitator (HLR) as a device that will make high quality CPR something anyone can do ‘with the push of a button.’

In reality, deploying and applying even the most automated and technologically sophisticated HLRs will require more skill and expertise on the part of EMS personnel, not less.
Mechanically delivered ACD-CPR is also more effective than conventional mechanical CPR, even when delivered per the new AHA standards. As an example, coronary and cerebral blood flows during LUCAS CPR are improved by 25-30% over those obtained with the Michigan Instruments Thumper HLR.
Steen S, Liao Q, Pierre L, Paskevicius A, Sjöberg T. “Evaluation of LUCAS, a new device for automatic mechanical chest compression and active decompression for cardiopulmonary resuscitation.” Resuscitation. 2002; 55: 289-299.
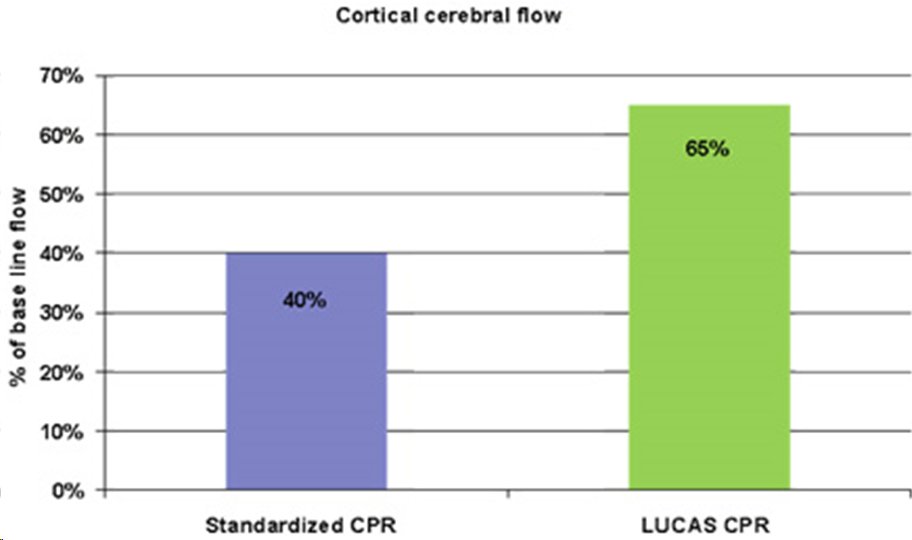
Rubertsson S, Karlsten R. “Increased cortical cerebral blood flow with LUCAS, a new device for mechanical chest compressions compared to standard external compressions during experimental cardiopulmonary resuscitation.” Resuscitation 2005; 65: 357-363
But of even greater interest in the context of cryopatient Transport is the dramatic improvement in the durability of perfusion being demonstrated with ACD-CPR using the LUCAS, as opposed to what can be achieved with conventional CPR. While mean arterial pressure (MAP) and cardiac output (CO) are often adequate to maintain cerebral viability during the first minute or two of chest compressions, they rapidly fall to levels that are inconsistent with survival thereafter. Deterioration of cardiac preload, rapid and progressive loss of chest wall elasticity (and thus recoil) and possibly elevated intrathoracic pressure from ‘auto-PEEP’ (gas trapping at the end of expiration and dynamic hyperinflation of the lungs) all likely contribute to the rapid decay in mean arterial pressure (MAP) and perfusion seen in conventional CPR.
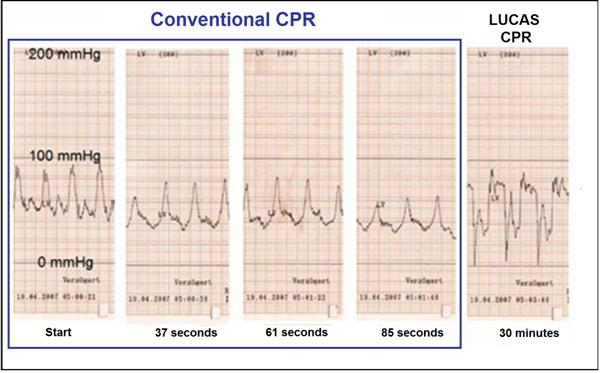
ACD-CPR using the LUCAS preserves MAP and perfusion, even during prolonged CPR; in one case up to 240 minutes. The representative waveforms above are from LUCAS CPR performed on 13 patients who experienced cardiac arrest during cardiac catheterization and who underwent CPR for times ranging from 45 to 245 minutes. Mean systolic and diastolic blood pressure were 81±23 and 34±21 mmHg, respectively; pressures fully compatible with preservation of brain viability and long-term survival.
Compressed Gas Bottles & the Autopulse
Aside from the problem of interrupting CPR while HLRs are applied, and the historically complex and clumsy nature of the devices, the other major barrier to the use of mechanical CPR has been the need for a bulky and heavy supply of compressed gas to power the devices. Typically, two E-cylinders containing 640 liters of oxygen or air will run an HLR for only 15 to 20 minutes. This is a major logistic hurdle in conventional emergency medicine which becomes far more serious in the setting of cryopatient Transport. Oxygen (compressed or in chemical form in ‘oxygen generators’ of the type used in commercial jetliners) cannot be transported on commercial aircraft nor shipped by common carrier because of the hazard it represents. As a result, cryonics Standby/Transport teams must find a way to acquire compressed gas immediately upon landing – something that is becoming increasingly difficult since the advent of electrically powered oxygen concentrators which have largely eliminated the need for 24/7 home delivery of oxygen in high pressure cylinders.
One solution to this problem was the development of the Autopulse (Zoll Medical Corporation) which is a battery powered HLR that delivers vest CPR. While vest CPR has been shown to be superior to conventional CPR in some studies, it lacks the ability of ACD-CPR to dramatically reduce intrathoracic pressure and to maintain MAP and CO during long duration CPR. An additional problem with the Autopulse for cryonics is that the device contains the electronics; control circuitry, motors and associated mechanical devices used to power and operate it which are located in the backboard that the patient rests upon.

Since cryopatients are immersed in ice water, this means that the device must be extensively re-engineered for this application. Suspended Animation, Inc., of Boynton Beach, FL has reportedly developed such a portable ice bath (PIB) compatible Autopulse which they have patented and plan to market to the cryonics community at a considerable mark-up over the Autopulse’s already high retail price of ~$20,000. Another problem facing the Autopulse is the increasing gap in the quantity and quality of both the published animal and human clinical research between the Autopulse and ACD-ITD-CPR. The strong selling point of the Autopulse has been its ability to operate on compact batteries for up to 20 minutes with the ability to rapidly and easily change out batteries without any interruption in CPR.
I Sing the LUCAS Electric!
A few months ago, LUCAS announced what has certainly been a long and desperately desired advance in HLR technology – in and out of the cryonics community. LUCAS is now marketing the LUCAS 2, which is a completely battery powered version of their pneumatically driven LUCAS 1 machine.

This second generation LUCAS uses the basic, the well-proven LUCAS 1 platform, with a number of potentially critical added improvements. In addition to using microprocessor controlled electronic actuators, the device contains a ventilation reminder; with plans to allow interface of the device to a sophisticated, compact ventilator in the near future. Most importantly, the LUCAS 2 operates for 45 minutes on the on the newly available lithium ion polymer (LiPo ) battery technology (with no test-cycles or reconditioning required) and may also be connected to and operated from electrical power points (wall outlets) or car outlets. The battery is neatly integrated in the hood of the HLR and it can easily and rapidly be changed out, making the LUCAS 2 a lightweight and compact device to store and carry (17 kg, complete).
Incredibly important to cryonics operations is the fact that the device uses a softer start during the initial adjustment to the patient’s chest, and is much quieter when in operation. This latter consideration is of critical importance in institutional settings where the noise generated by pneumatically driven HLRs has resulted in significant resistance (and even refusal to allow their use in a few cases) on the part of hospital, extended care facility, and hospice administrators. The LUCAS 2 should go a long way towards overcoming this problem since the noise level is actually less than that often encountered when conventional manual CPR is administered.

The LUCAS user interface remains very simple with fingertip access to all operating modes and 3-step, 3-button actuation. Delightfully, the LUCAS 2 can operate from wall current (100-240V / 50/60 Hz) or from an automobile car outlet (12-24V); if the engine is running to power the vehicle alternator, the unit can operate from the vehicle power supply indefinitely (or as long as the petrol supply lasts)!