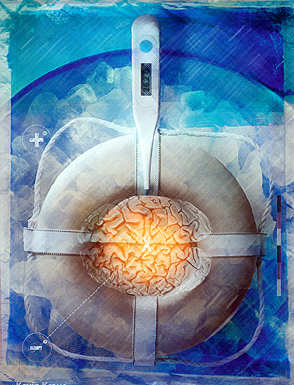
Prospects for Mild Therapeutic Hypothermia and Improved CPR in Cardiopulmonary Cerebral Resuscitation
 There are two kinds of hypothermia: protective or preservative hypothermia, and therapeutic hypothermia. The former is easy and straightforward to understand for most, clinicians and laymen, alike. However, therapeutic hypothermia has proved to be a far more difficult idea to communicate, probably because it is so easy to conflate it with protective hypothermia.
There are two kinds of hypothermia: protective or preservative hypothermia, and therapeutic hypothermia. The former is easy and straightforward to understand for most, clinicians and laymen, alike. However, therapeutic hypothermia has proved to be a far more difficult idea to communicate, probably because it is so easy to conflate it with protective hypothermia.
Anyone who has had any contact with refrigeration will at once understand the concept of protective hypothermia. Foodstuffs, and other biological materials that are cooled, experience protection against spoilage and decay roughly in proportion to the degree to which they are cooled. A little cooling slows decomposition a bit, and enough cooling will stop it altogether. Again, the temperature-induced decrease in the rate of chemical reaction is a fundamental property of chemistry which is understood intuitively by anyone who lives where it gets cold, or where refrigeration is in use.
By contrast, therapeutic hypothermia does not rely primarily upon the slowing of metabolism or the rate of chemical reactions that occurs as a result of cooling, but rather upon the effects very modest degrees of cooling have on gene activation and signal transduction in mammals. Controlled, mild therapeutic hypothermia (MTH) is generally understood to constitute a reduction in body temperature from ‘normal’ for the species being treated, to 3oC below normal. In the case of humans, this would mean a reduction in body temperature from 37oC to 34oC. Such a modest reduction in temperature results in profound down-regulation of pro-inflammatory cell-signaling pathways and causes the inactivation of genes involved in a multiplicity of deleterious cellular and systemic processes. Similarly, MTH can inhibit apoptosis of brain cells, and slow or halt the downward spiral of excessive metabolic demand by injured cells, causing yet more non-productive hyper-metabolism, and consequently even more cell death. In this article, the biomechanics of MTH are briefly explored, as well as the prospects for improved outcomes in patients who suffer anoxic-ischemic brain injury as a result of cardiac arrest as a result of the rapid application of MTH following the insult.
Read the complete paper in PDF here.